Thinning Post-CXL: How was it managed?
A 21-year-old male came with complaints of blurring of vision with a history of eye rubbing. He had bilateral keratoconus, worse in the left eye than the right.
Corneal topography & Pentacam examinations showed keratoconus in both eyes, more advanced in the left. With a central corneal thickness of 465microns, patient underwent Corneal Collagen Cross Linking in the left eye first which was the worse eye. He underwent the conventional Dresden protocol.
Over the next few years, we could see progressive thinning and fluctuation in his pachymetry and progressive flattening in his keratometry.
He was advised use of Rose K lenses as well as deep anterior lamellar keratoplasty. But he was not keen on both.
Months later, the patient presented with blurring of vision in the left eye.
He said dust went inside his left eye and he rubbed it after which his vision had become blurry.
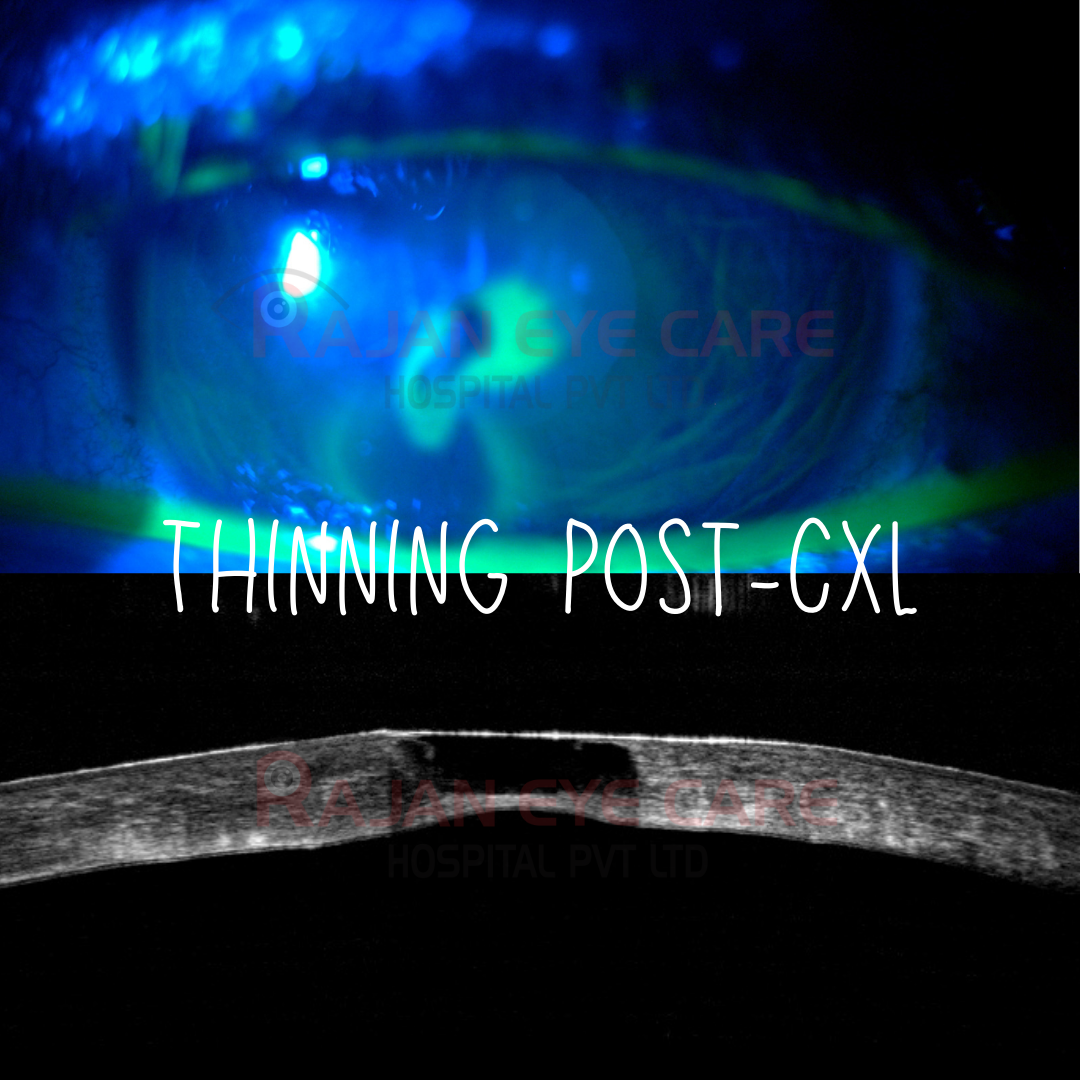
This trivial trauma had caused a corneal perforation confirmed by Seidel’s test and AS-OCT confirmed a corneal perforation
Immediate tectonic temporization was done using cyanoacrylate glue and a bandage contact lens
Once the eye stabilized, A deep anterior lamellar keratoplasty was performed for visual rehabilitation
Patient is doing well with a vision of 6/9 at present
This case is a clear example of how the effects—and limitations—of corneal cross-linking can declare themselves many years after the procedure
It underscores the importance of long-term surveillance, including regular follow-up with serial Pentacam imaging, and continuous reinforcement of behavioural counselling, particularly strict avoidance of eye rubbing
www.ophthalmobytes.com
Image from Rajan Eye Care Hospital
#ophthalmology #ophthal #doctor #health #medical #vision #education #optometry #medicalstudent #optometrist #medicine #eye #ophtho #ophthalmologist #ophthalmo #med #medicaleducation #ophthalmologyresident #ophthalmologyresidency #apaoyo #cornea #keratoconus #collagencrosslinking #perforation #asoct #seidelstest